Retinal Laser Surgery
Retinal laser surgery is used to treat a variety of problems including retinal tears, retinal holes, small retinal detachments and leaking blood vessels in the back of the eye. The laser generates a light source that is directed through a special contact lens or ophthalmoscope. As the light reaches the problem area to be treated, it begins to heat up. The body responds to heal the area and in so doing, a seal is created. Laser surgery is frequently performed in the office of the surgeon, but it is also utilized during other complicated retinal procedures in an outpatient surgical area.
Retinal detachments, holes and tears
 Retinal detachments, holes and tears are serious conditions that require immediate attention.
Retinal detachments, holes and tears are serious conditions that require immediate attention.
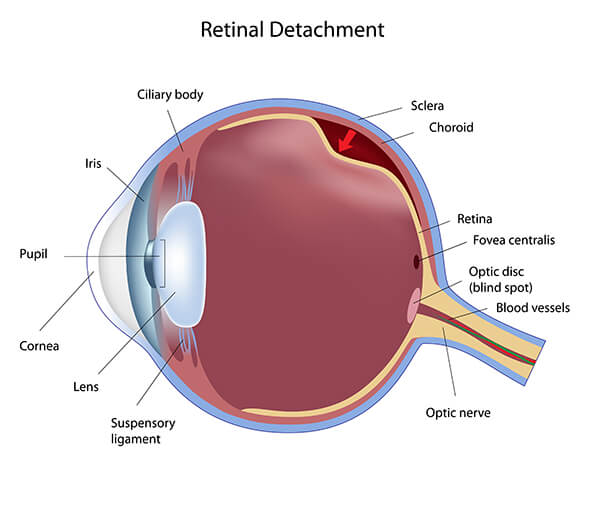
A retinal detachment occurs when the retina separates from the back wall of the eye. This typically happens when liquefied vitreous fluid passes through a small tear in the retina and collects behind the retina. This collection of fluid causes a lifting action and markedly disturbs the vision. Frequently, detachments begin with loss of peripheral vision and patients may notice a dark shadow, or a veil, coming from one side, above or below. Left untreated, in most cases, after a retinal detachment starts, the entire retina will eventually detach and all useful vision in that eye will be lost.
What is the treatment for a retinal detachment, a retinal hole or a retinal tear?
The retinal surgeon will decide the most effective treatment for a retinal detachment, hole or tear. If a retinal detachment or tear is small, it may be repaired using laser surgery, cryotherapy (freezing an area), or a combination of the two. If a detachment becomes too large for the laser treatment or cryotherapy alone, surgery is normally necessary to reattach the retina. Without surgery, vision will almost always be completely lost. There are three types of surgery for retinal detachment: 1) scleral buckling surgery, 2) pneumatic retinopexy, and 3) vitrectomy.
Scleral Buckling Surgery
Considered the traditional surgery for retinal detachments, scleral buckling is performed using local, and in some cases, general anesthesia. The first step in this procedure is treatment of the retinal tear by use of cryotherapy, or freezing. The surgeon places a cryoprobe on the outside of the eye, and then, using a special instrument to look into the eye, the surgeon correctly places the cryoprobe in the vicinity of the retinal tear. The freezing action of the cryoprobe causes scarring to occur. A piece of silicon plastic is then sewn onto the outside of the eye in this same area, thus causing the eye to buckle (hence the name of the surgery) inward and holding the retina against the treated area. The scarring from the cryoprobe seals the retinal tear. The silicone buckle is left permanently in place after the surgery.
There are a variety of options that surgeons may use based upon the specific condition of the retinal detachment once it is observed from within the eye. In some cases, the retinal surgeon may place a silicon band around the entire circumference of the eye. By doing so, this reduces the pulling effect that the vitreous (fluid portion of the eye) may be placing upon the retina. The surgeon may also make a small opening in the outer wall of the eye to allow fluid to drain from behind the retina, thus improving the chances of the retina reattaching successfully. In other cases, the surgeon may inject a gas bubble directly into the vitreous cavity. After the surgery has been completed, the patient will then be positioned such that the gas bubble rises to push the retinal tear against the scleral buckle to help ensure the tear remains closed and heals.
Success rates for reattaching a retina are generally better than 80% when only one operation is required. Additional operations can improve the success rate to over 90%. Unfortunately, good vision does not automatically follow a successful retinal reattachment. Usually, the status of the macula (central portion of the retina) during the retinal detachment will be the best predictor of restoring good vision. If the macula was detached at any time during the retinal detachment, vision rarely returns to normal, however it can improve. In this instance, it may take several months before the best vision is achieved. Regrettably, even when the macula remains attached and the retina is successfully reattached, some vision can be lost.
What to expect after scleral buckle surgery
Patients that undergo scleral buckle surgery typically experience redness and slight soreness in their eye for about a month or two. The operated eye may experience watering for several weeks so a patch may be preferred. Patients should expect vision to be blurry following surgery; in some cases this may last for weeks. Patients will also report a scratchy and itchy sensation that is a result of the stitches used to close the outside of the eye. It is not normal to experience severe pain and this should be reported to the surgeon immediately. Medications after surgery usually include antibiotic drops to prevent infection and drops to increase the comfort of the eye. On occasion, a patient may stay overnight in the hospital following this surgery, but generally they are released on the day of surgery.
During the weeks that follow scleral buckle surgery, the surgeon will follow you closely to ensure that the retina remains attached. Your physical activities will be limited during this period. Frequently, you may need to have new glasses made since the scleral buckle alters the shape of the eye. Should the retina redetach, your surgeon would discuss the options available for a reoperation.
Pneumatic Retinopexy
Pneumatic retinopexy involves the intraocular injection of an inert gas bubble to press on the retina and seal the retinal break. The characteristics of the retinal tear, typically the size of the tear, will often dictate whether the surgeon would recommend this procedure. The advantages of this procedure include local anesthesia and the avoidance of the cutting that occurs with a scleral buckle.
As in the scleral buckle procedure, the retinal tear is first sealed using either a laser treatment or cryotherapy (freezing). Once the gas bubble has been injected in to the vitreous cavity of the eye, the patient’s head is then positioned face down such that the bubble rises and pushes the detached retina in the area of the tear against the back wall of the eye, thus allowing it to reattach. The surgeon will decide how long the patient must remain in a fixed position, but this can take several weeks and often requires some specialized equipment to help maintain lifestyle functions. Compliance with positioning is mandatory for the success of the procedure. In fact, failure to comply with proper positioning could lead to other complications such as cataract or increased eye pressure. During the recovery phase of two to six weeks, no airplane or high altitude travel is allowed because of the high altitudes could cause an expansion in the gas and the increased pressure could damage the eye.
Vitrectomy
The most severe retinal detachments are typically treated by vitrectomy which consists of the removal of the liquid, gelatinous mass that fills the rear two-thirds of the eye between the lens and the retina. This surgery is performed under local or general anesthesia. The vitreous is replaced with either clear fluid or a gas that completely fills the eye. The eye does not replace the vitreous gel itself, but lack of vitreous gel does not affect the ability of the eye to function properly. The surgeon may frequently use any combination of treatments including laser and scleral buckle in together with the vitrectomy. Air, gas or silicone oil may also be injected into the eye to assist in holding the retina in place while reattaching it to the back wall of the eye. As with pneumatic retinopexy, the patient may be required to assume a face-down position for a period of time after surgery. If silicone oil is used, it may need to be removed with a different surgical procedure at a later time. Because of the complicated nature of this surgery, vitrectomy and associated procedures usually last one to two hours (even longer for more severe cases). Patients report feeling some discomfort after surgery often describer as a scratchy feeling. Significant pain is uncommon and should be reported to the surgeon immediately.